

This represents reperfusion of the injured tissue. The T waves in the anterolateral leads are all inverted.
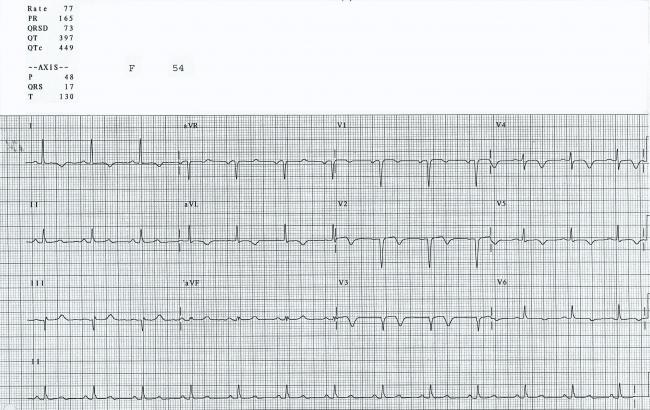
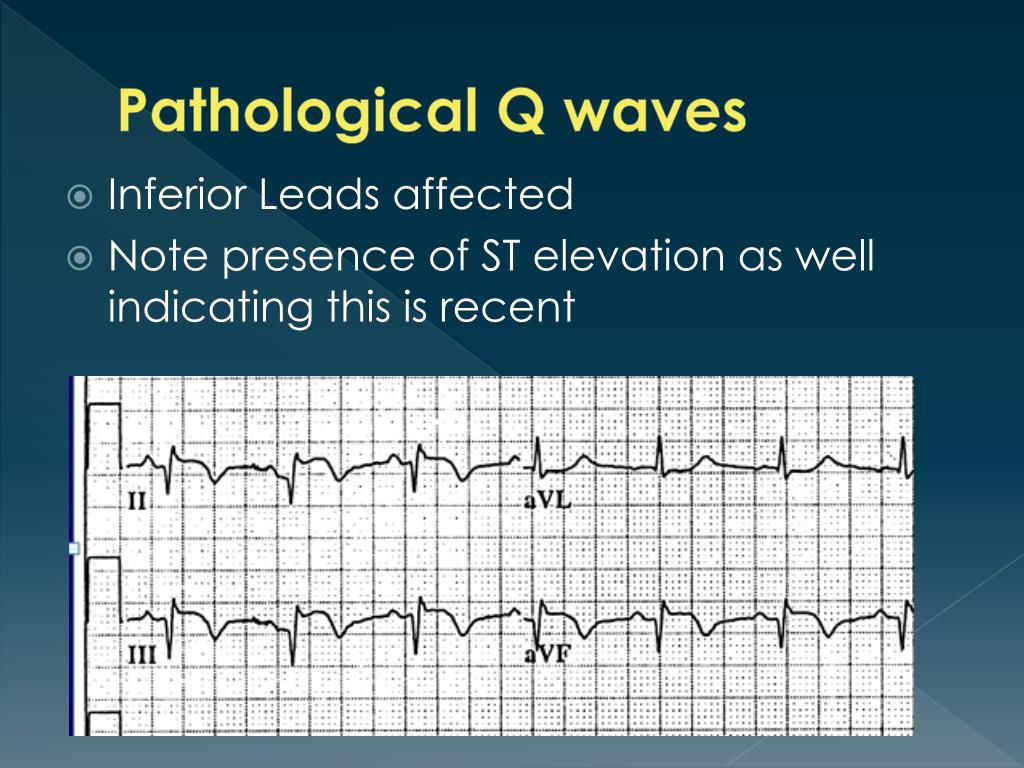
This shape is usually abnormal, and it has persisted even though the acute injury is subsiding. While they are no longer elevated (the acute injury is over), they are flat and almost convex upward. What ST and T wave changes are present? All of the leads listed above show a flattening of the ST segments. This area is perfused by the left coronary artery, and she had a proximal lesion. The precordial leads reflect the anterior and low lateral walls of the heart, and Leads I and aVL show us the high lateral wall. Where was this M.I.? The affected leads are all of the precordial leads (V1 through V6), as well as I and aVL. Her ECG shows the signs of healing injury, as well as probable permanent damage. She did not receive interventional treatment, as it was not available where she lived when this happened years ago. This ECG is from a 54-year-old woman who had an M.I. It is also difficult to determine ST and T wave changes in the PVCs for the same reason. The axis of the sinus beats is around 60 degrees (normal), but the axis of the premature beats is difficult to determine due to the low voltage and biphasic QRS complexes in the frontal plane leads. The ECG signs that the ectopic beats are ventricular are: lack of P waves associated with the premature beats, QRS width about. By the end of the strip, the underlying sinus rhythm has slowed slightly. Every other sinus beat is obscured by the PVCs. After the second sinus beat, ventricular bigeminy occurs. The patient expired before any further diagnosis was made.ĮCG Interpretation The rhythm is sinus at a rate of about 80 bpm (first two beats). Electrolytes were monitored and corrected when necessary. He continued to have occurrences of non-sustained ventricular tachycardia (VT), progressing to sustained VT. Ten days post PCI, the patient had ventricular arrhythmias and went into cardiac arrest, but was resuscitated. He underwent primary percutaneous coronary intervention (PCI) of the proximal left anterior descending coronary artery (LAD). He was rated Killips Class 1 (no evidence of congestive heart failure), TIMI risk score 4 (14% risk of all-cause 30-day mortality). Hospital Course He was diagnosed with anterior wall STEMI and taken to the cath lab. He had a history of hypertension, 40 pack-year smoker. The Patient This ECG was obtained from a 51-year-old man who presented to EMS with acute chest pain. Read more about Right Bundle Branch Block With Probable Previous M.I.The J points in this ECG all appear to be at the baseline, with no overt STEMI. Occasionally, the terminal delay – especially in Leads III and aVF – can be mistaken for ST elevation. Right bundle branch block can make evaluating for ST segment elevation a bit tricky. It would, of course, help to know this patient’s history. that would have caused these Q waves is old, as there are no acute ST changes. However, the probability of pathological Q waves in the inferior leads offers a more likely explanation for the leftward axis shift. Lead II will be very small, or flat, or negative. LAH causes a frontal plane axis shift – instead of Lead II having the tallest QRS of the limb leads, Leads I and aVL will be the tallest upright QRS complexes of the six limb leads. The left anterior fascicle has the same blood supply as the right bundle branch. It is not unusual for people with RBBB to also have a left anterior hemiblock (LAH), also called left anterior fascicular block. It is normal for the T waves to be in a direction opposite that of the terminal wave (inverted in Leads V 1 and III, for example.)
This delay can be seen in every lead, but is especially easy to see in Leads I and V 6, where there is a wide little s wave. This terminal delay widens the QRS without affecting the depolarization or contraction of the left ventricle. The R prime (R’) represents the right ventricle depolarizing slightly after the left ventricle. The QRS is wide at 148 ms (.148 seconds). We see the right bundle branch block (RBBB) pattern: rSR’ in the right precordial leads (with a tiny q wave in V1, which is not typical of RBBB). There is a first-degree AV block, with a PR interval of 232 ms. This is a good opportunity to teach the value of evaluating rhythm strips in more than one simultaneous lead, as subtle features may not show up well in all leads. We suggest Lead I to best view the P waves in this example. The P waves are small, and difficult to see. So, it is normal sinus rhythm, but the rate is probably not “normal” for this patient. We have no other clinical information.ĮCG Interpretation The rhythm is regular and fast, with P waves, at 95 beats per minute. This ECG was obtained from an 87-year-old man with chest discomfort.


 0 kommentar(er)
0 kommentar(er)
